Shorter hospital stays, fewer complications in response to treatment, and improved patient satisfaction. Evidence-based practice isnât just a theoretical concept; it has real-world benefits. When nurses invest their time and effort in using research-based evidence to guide their decisions and practices, they tend to see positive results. In fact, a recent scoping review published in Worldviews on Evidence-Based Nursing found that, in cases where clinicians used evidence-based practices, metrics ranging from recovery time to cost efficiency improved about 94% of the time.
Developing an in-depth understanding of evidence-based practice in nursing can serve as an important first step for clinicians and aspiring clinicians seeking to incorporate it into their practice. Nursing programs can provide the comprehensive education practitioners need to unlock the full potential of evidence-based practice.
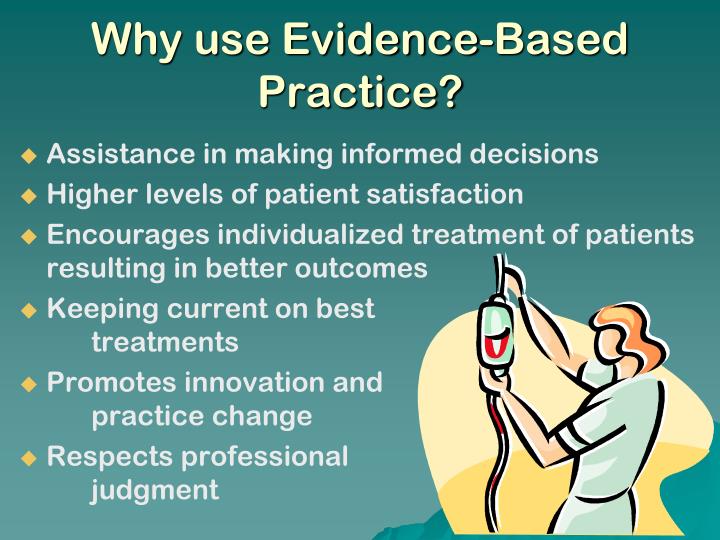
Evidence-based practice (EBP) has become an integral part of quality nursing care and positive patient outcomes. As nurses, implementing EBP allows us to provide the highest quality care to our patients by ensuring we are using the most up-to-date and relevant evidence. In this article, we will explore the top 10 benefits of evidence-based practice in nursing.
1. Improves Patient Outcomes
One of the most significant benefits of EBP is that it leads to improved patient outcomes. When care is guided by the best clinical evidence patients experience fewer complications, faster recovery times and better overall health. For example, research shows that implementing EBP techniques to prevent hospital-acquired infections can reduce infection rates by up to 70%.
2. Provides Higher Quality Care
EBP ensures that patient care is based on the most current research, clinical expertise, and patient preferences. This results in the delivery of higher quality care. Nurses can be confident they are using techniques and treatments that are supported by evidence, rather than just tradition or intuition.
3. Encourages Critical Thinking
The EBP process requires nurses to find and appraise evidence, assess its validity, and determine how it applies to patient care. This process enhances critical thinking as nurses must evaluate research studies, use logic and reasoning to interpret findings, and synthesize information. These skills lead to improved clinical judgment and decision making.
4. Promotes Interprofessional Collaboration
Implementing EBP requires collaboration between nurses, physicians, pharmacists, physical therapists, and other members of the healthcare team. Working together gives various perspectives on treatment options and care plans, resulting in the best evidence being used. This interprofessional approach has been shown to enhance patient satisfaction and health outcomes.
5. Keeps Nurses Up-To-Date
The knowledge required for quality nursing care is constantly evolving as new research emerges. EBP ensures nurses stay current about best practices and new treatment options. Implementing EBP introduces nurses to cutting edge evidence that would otherwise take years to filter into practice.
6. Reduces Health Care Costs
The use of up-to-date evidence helps prevent medical errors, inappropriate or unnecessary treatments, and other inefficiencies that drive up costs. For example, EBP techniques to reduce hospital-acquired infections save thousands in additional treatment. Preventing readmissions through EBP also generates significant healthcare savings.
7. Increases Patient Satisfaction
Patients experience greater satisfaction when they know their care is based on science and quality improvement. EBP leads to better communication between providers and patients, increased patient education, and care that aligns with patient values and preferences. This patient-centered approach is crucial for high satisfaction scores.
8. Improves Care Consistency
Variation in care between providers, units, and facilities can lead to uneven quality and outcomes. EBP helps reduce this inconsistency by promoting standardized best practices based on evidence. This consistency in nursing care supports optimal patient outcomes across the entire healthcare system.
9. Facilitates Continued Learning
The EBP process promotes continued reading, research, and learning for nurses. Staying caught up on the latest evidence requires ongoing education and a commitment to improve knowledge. EBP transforms nursing into an evidence-based learning profession.
10. Strengthens Record Keeping
Clear, comprehensive documentation is key to EBP implementation. Nurses must record details about assessments, treatment rationale, patient response, and more. Strong record keeping promotes information sharing for collaborative decision making and evaluation of care effectiveness.
The Importance of Evidence-Based Practice in Nursing

Shorter hospital stays, fewer complications in response to treatment, and improved patient satisfaction. Evidence-based practice isnât just a theoretical concept; it has real-world benefits. When nurses invest their time and effort in using research-based evidence to guide their decisions and practices, they tend to see positive results. In fact, a recent scoping review published in Worldviews on Evidence-Based Nursing found that, in cases where clinicians used evidence-based practices, metrics ranging from recovery time to cost efficiency improved about 94% of the time.
Developing an in-depth understanding of evidence-based practice in nursing can serve as an important first step for clinicians and aspiring clinicians seeking to incorporate it into their practice. Nursing programs can provide the comprehensive education practitioners need to unlock the full potential of evidence-based practice.
Accessing and Evaluating Evidence ¶
Nurses can access evidence through various channels, including peer-reviewed journals, online databases, and professional organizationsâ guidelines. By critically evaluating the quality and relevance of the evidence, nurses can determine which studies may apply to their patient populations and clinical settings.
What is Evidence-Based Practice?
Why is evidence-based practice important in nursing?
EBP is essential as it aims to provide effective, relevant care focused on improving patient outcomes and strengthening the nursing profession. Understanding evidence-based practice in nursing + 10 examples, like those featured in this article, is crucial for the success of nurses. 1. What Did Nurses Do Before Evidence-Based Practice?
What is evidence-based practice (EBP)?
Evidence-based practice (EBP) is defined by Duke University Medical Center as “the integration of clinical expertise, patient values and the best research evidence into the decision-making process for patient care.” EBP strategies allow nurse practitioners (NPs) and other health care providers to translate research findings into clinical practice.
What is evidence based nursing?
Although evidence based nursing relies on research, it also considers the desires of individual patients. Since one of the main tenets of nursing is focusing on the patient’s needs, evidence based practice helps you continue to improve patient outcomes while weighing the preferences and experiences of each patient.
Does evidence-based practice improve patient outcomes?
BMC Nurs. 2021; 20: 13. Integrating evidence-based practice (EBP) into the daily practice of healthcare professionals has the potential to improve the practice environment as well as patient outcomes. It is essential for nurses to build their body of knowledge, standardize practice, and improve patient outcomes.